Decoding the Spectrum
Could autism be diagnosed with a simple blood test? For one GW biochemist, the quest is personal.
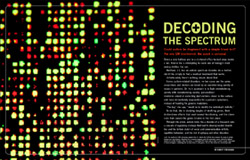
The results of a DNA microarray analysis from Dr. Valerie Hu's GW lab that compare the levels of activity between two sets of genes. Visualized by a computer program, each dot represents a gene, colored to indicate whether its activity is higher, lower, the same, or nonexistent (the black spaces) than a control sample. Forty-eight of these rectangles—containing info on more than 41,000 genes—fit on a few inches of a microscope slide.
William Atkins
Down a side hallway and in a cluttered office tucked away inside a lab, Valerie Hu is attempting to crack one of biology's most vexing riddles: her son.
Matthew, 23, has an autism spectrum disorder. As a mother, she'd like simply to find a medical treatment that works.
Unfortunately there's nothing simple about that.
Across autism-related disorders, no two cases are the same; researchers and doctors are beset by an overwhelming variety of issues in patients. Dr. Hu's approach is to fight overwhelming variety with overwhelming variety: personalized medicine aimed at correcting dysfunctions closer to the surface and more immediately responsible for a person's symptoms, instead of hunting for genetic mutations.
"The key," she says, "would be to identify the individual's deficits."
To do that, she is studying tangles of misfiring genes, their trickle-down effects that snarl normal functioning, and the chemicals that caused the genes trouble in the first place.
Through this prism, autism looks like a disorder of a thousand cuts: a cascade of regulatory mishaps that lead to developmental disabilities and the telltale clutch of social and communication deficits, repetitive behaviors, and the risk of epilepsy and other disorders.
One in 110 children in the United States, on average, is affected by autism; boys four times as often as girls. There is no cure, and treatments can be hit-or-miss.
"The problem is: Right now we're just guessing," Dr. Hu says of the efforts to treat Matthew. "I'm still puzzled."
Her recent research, though, is adding to insights that are bringing scientists and the public tantalizingly close to the idea that medicine might soon have a better shot at relieving, or even reversing, the individual features of autism—like a thousand Band-Aids for those thousand cuts.
Even as the promise of such treatments remains beyond arms' reach for now, her work might be closing in on the next-best thing. Early detection and behavioral intervention currently are the best hope for an autistic child, and Dr. Hu thinks she may be nearing "the Holy Grail" for her line of work: a means of diagnosing autism with a simple blood test.
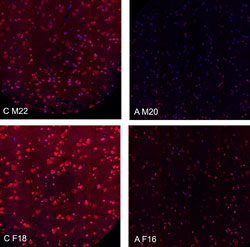
The brightness of the pink spots in this image, from yet unpublished data, shows a stark difference in levels of an important protein in brain tissue belonging to healthy controls (left) and autistic individuals (right). The low levels in the brain correspond with Dr. Hu's findings from blood-derived cells, lending further support to her idea that these cells may be an accurate window into the brain.
Courtesy of Valerie Hu
Dr. Hu's office in the GW Medical Center is a stereotypical scholar's workshop: Mounds of paper crowd her desk (and a second desk, and parts of the floor), and books on chemistry and biology climb the walls.
It's the pictures all around, though, that speak volumes: photos of family, of grinning golden retrievers, and most significantly of Matthew—as a child and through the years leading up to him in cap and gown for high school graduation in 2006.
Her pride is evident, though "it was such a struggle," she recalls.
Back in 1989, Dr. Hu and her husband, David Smith, had taken their 2-year-old son to the doctor with concerns that he wasn't yet speaking. Six months and several tests later Matthew was diagnosed with Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), one of the several types of autism.
(Even over time, though, the lines between different types can be blurry: Later Matthew also would be characterized as fitting the bill for Asperger syndrome.)
In hindsight, there had been other signs that something was amiss.
Dr. Hu recalls reading to Matthew from a children's book and at a certain page he wouldn't let her move on. "He always wanted to look at some little animal character there that was having chamomile tea," she says with a laugh. "He couldn't get past it. But now I think you might recognize that as a sign that there's something you'd better check."
The diagnosis offered little relief. "PDD-NOS doesn't tell you anything," she says. "'Not otherwise specified' means 'we don't know.'" And it was uncharted territory for her as a parent and a researcher. Dr. Hu had joined the GW faculty the year before as a chemist working with cell membranes, but she was more than a decade away from hatching a career in autism.
She found little on PDD-NOS in the medical literature. And the more she read about autism, in general, "the more depressing it was, because the prognosis for anyone with autism was pretty bleak."
She and her husband looked inward for blame, a fruitless effort.
The energy, anyway, was better spent on being a parent. "From the time he got a diagnosis, your life changes, honestly. Because all you're thinking about is, 'What can I do to help my kid?'"
For years those efforts would be outside the lab, trying to keep Matthew from slipping through the cracks at school, which Dr. Hu says is common for kids at the high-functioning end of the autism spectrum.
In preschool, even though Matthew was grouped with kids who had other disabilities, theirs did not affect social skills. So when the teacher would come around with a Big Bird puppet and interact with the children, "most kids loved it," recalls Dr. Hu. "But Matt would kick at it."
He transferred into a specialized preschool program for kids with autism and made swift advances, to the delight of his parents. But Matthew would labor intensely the rest of the way through the public school system; too intelligent and high-functioning to be grouped with students with learning disabilities, too socially impaired to fit in with mainstream classes.
Along the way Dr. Hu helped establish a support group in Montgomery County, Md., for local parents of kids with Asperger syndrome and other types of high-functioning autism; the group did bring about changes at school, she says, though not soon enough to help Matthew.
At the end of 2004 she took a sabbatical and used that time to shift into a career in autism research. It was "a no-brainer," she says—probably the last easy answer she'll encounter in this journey.
The vast majority of autism cases are diagnosed only by observing a child's behavior as it develops in the first few years of life. Milder cases of autism can take even longer to fully surface.
In these cases of so-called idiopathic autism (arising from no known cause) a child's behavior offers the only clues to what's going on inside the brain. Medical diagnostic tests don't exist for idiopathic autism—accounting for perhaps 80 percent or more of the cases—because researchers haven't been able to figure out what to look for.
"Each individual has a different constellation of genes that are affected," Dr. Hu says. For example, "a lot of the genes that have been identified by genetic analyses have been pointing toward the synapse—where nerve cells come together, where they establish connections. But a given individual probably has several of those genes that are impaired, and not the same genes as different individuals.
"So the question is: How do you account for that kind of disorder?"
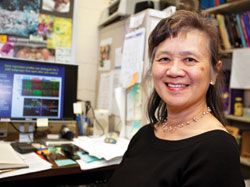
Researcher Valerie Hu is plumbing the mysteries of autism in hopes of finding a way to pinpoint personalized drug targets that will ease an individual's symptoms, including those for her son, Matthew.
William Atkins
For Dr. Hu, it means panning back to take in a broad view of the body's biological systems—where have things run amok, even if we don't know why.
These biological systems run like a network of connected highways: a rush-hour wreck in one lane can foul an entire route and spread to the roads around it. By better understanding how molecular traffic moves on these highways, Dr. Hu's hope is that her research will lead to fixes that keep traffic running smoothly, even if the ultimate roots of the problem remain unknown.
"And that's what the field absolutely needs at this point," says Jacqueline Crawley, an autism researcher and chief of the Laboratory of Behavioral Neuroscience at the National Institute of Mental Health, in Bethesda, Md. "One can develop a treatment without completely understanding how it works, what the mechanism is biologically."
"The kind of gene discovery that Valerie is doing is often called hypothesis-generating," says Dr. Crawley, "so she comes up with the gene profiles and there's some very interesting genes that pop out, and then those become potential targets for treatment development."
Dr. Hu's highway road work involves understanding the genes—sections of DNA that are turned on and off, producing proteins that help build and regulate cells in the body—as well as the function of genes along the complete set of DNA, called the genome.
Her approach also involves an understanding of the epigenome, which scientists are only beginning to fully grasp. Just as genes control protein production, the epigenome can control the on-off switch of genes using natural and manmade chemicals. And like the genome, the epigenome can be inherited.
"I jumped in feet first," Dr. Hu says. "I didn't have any funding, I hadn't done any work on autism prior to this, I didn't have a track record."
Nevertheless her initial effort, in 2006, was one of the first studies to explore differences in gene expression—that is, the activity of genes—in autism. She was able to do this by comparing a small group of identical twin pairs and their siblings. Identical twins have the same DNA, and DNA between siblings is very similar, making it easier to find differences in gene expression between an autistic twin and a nonautistic twin or sibling, or even differences between autistic twins with different symptoms.
And rather than looking for these changes in brain tissue, Dr. Hu's study was done using copies of blood cells, called lymphoblasts, that were grown in a lab. While brain tissue is the gold standard for this kind of autism research, it's difficult to come by, and Dr. Hu figured future diagnostic tests would rely on bodily tissue that's much more accessible. (Cheek swabs and saliva, she says, yield too few cells.)
Demonstrating for the first time that differences relevant to autism may be visible in cells outside of the brain offered the hope that the brain might be glimpsed through a window rather than requiring a trip down the chimney.
(This year she added strength to that concept: Again looking at a small group of twins and siblings, she showed that the decreased activity of two genes—one of which had not yet been linked to autism—in lab-grown autistic cells was mirrored in autistic brain samples.)
The big question remained—and yet remains—just how useful these cells can be in identifying genes and pathways to treat in autism, and in identifying biological hallmarks that can be used to make a diagnosis. The first step in making sense of such a varied population was to "divide and conquer," as Dr. Hu calls it: separating autistic people into smaller, more similar groups based on behavior.
Analyzing data from standard behavioral tests on more than 1,950 autistic people, her lab fairly cleanly divided the group into four categories: those with severe language deficits; milder symptoms across the board; noticeable savant skills; and those of intermediate severity.
Using lab-grown cells, the team then looked at the level of gene activity among 87 autistic males from three of these groups (all except intermediate; the team wanted to test the concept by focusing on the extreme ends, Dr. Hu says). What they found was that beyond behavior, each group also could be categorized by a unique "signature" of gene activity when compared to each other and compared to a group of 29 nonautistic people.
"That was a big, important set of findings," says Dr. Crawley, of the National Institute of Mental Health, whose lab studies the behavior of mice genetically designed to mimic autistic symptoms. Elucidating so-called signatures, she said, could be instrumental to developing diagnostic tests and areas ripe for treatment.
The result is a list of each autistic group's genes that appear different from those of the healthy controls, with areas of overlap perhaps accounting for very common symptoms between groups.
Most curious, though, is a cluster of 20 genes that overlaps all three groups.
These are called "noncoding" genes, which often are involved in regulating other genes instead of producing proteins. But the functions—if any—for this group of 20 remain a mystery, Dr. Hu says.
Data from her study and others suggest many of them may be linked to how cells respond to male sex hormones, like testosterone, and could someday shed light on why males are so disproportionately prone to autism.
The study was the launchpad for what she hopes will be a diagnostic tool for autism.

Dr. Hu talks with Mindy Or, an undergraduate at University of Maryland, Baltimore County, who is working on a project in the lab this summer. Dr. Hu is known for hosting and helping student researchers from the Washington area on a regular basis.
Courtesy of Valerie Hu
In data that are not yet published, Dr. Hu says her lab was able to refine the slate of thousands of affected genes to sets of fewer than 30 that could be used to make a diagnosis. These sets were able to separate the autistic cases from nonautistic with roughly 90 percent accuracy, and when using sets of genes designed to look for each autistic subgroup the accuracy increased to 98 percent.
As of press time Dr. Hu had applied for patents on her work, and it had generated interest from several companies aiming to further develop the findings for use in diagnostic tests and treatment.
Much more work will need to be done to validate those results, says Dr. Hu, such as conducting the test with cells drawn directly from the blood (rather than lab-grown copies) and with a larger group of people. As Dr. Crawley, of the NIMH, points out: The road to a diagnostic test has been a long and arduous one that, at the very least, seems to have some pavement left to travel.
Still, even the immediate results from the study allowed Dr. Hu's lab to begin exploring the body's network of biological highways for speed bumps that may be ripe for treatment.
One example can be found in the severe language-deficit group. Among thousands of affected genes, several were involved in circadian rhythm (one of the body's internal clocks regulating the sleep cycle and hormone levels), which is tied to many symptoms of autism, including difficulty sleeping.
Isolating these very specific problems could lead a patient to simple fixes for the effects of misfiring genes. In the case of circadian rhythm, this might be something as simple as over-the-counter melatonin supplements.
"I'm not saying it's going to cure autism," Dr. Hu says, "but it might help with the sleep disturbance. And anybody who chronically can't sleep isn't going to function well, no matter what."
The sheer volume of genes gone awry in autistic individuals, she says, suggests the presence of "master switches that are turning the genes on and off." If so, harnessing these chemical switches might provide a more effective treatment that lightens or even curbs autistic symptoms at their roots.
Manipulating so-called epigenetic causes would tweak the expression of genes, like very finely tuning a stereo to just the right frequency. If they can be isolated and manipulated—no small task—they could prove easier to fix in the near term than deeper genetic mutations that may be at play in autism.
"It's not like you have to change the sequence of the DNA to correct the problem," Dr. Hu says. "You just have to alter the way the gene is used. So that's a big difference."
A pair of small studies from her lab this spring helped illuminate two elements of epigenetics: chemical tags called DNA methylation and microRNAs. The team found that, together, the two chemicals may have a hand in hundreds of the abnormally expressed genes they saw in the study's small number of subjects.
Drugs to reverse methylation already are used in cancer patients, Dr. Hu says, and levels of microRNA also can be controlled. But in order to parlay that to autism, much work remains in figuring out how to deliver treatments to precisely the right genes.
"We're not there yet, for sure," she says. "But there's a possibility."
Four-hundred-eighty-nine. That was the tally, reported last year, of the number of treatments and therapies in use by several thousand autistic children registered in an online survey. They ranged from applied behavior analysis, to speech and language therapy, to drugs, vitamins, special diets, and prayer. Some have been well-vetted, although the majority still are considered unfounded.
Writing in the newspaper Pediatric News, physician Paul Law, the director of the Interactive Autism Network at Baltimore's Kennedy Krieger Institute, noted that autistic kids in their survey were using an average of 5.2 treatments simultaneously.
Many used fewer. But one child was on a combination of 68 treatments.
The numbers hint at how much of an elusive target parents and researchers are up against.
Aside from Dr. Hu, more than two dozen GW faculty members are pursuing autism from myriad angles—from studies of the brain and art therapy treatments to health policy analysis. And planning began this year for an autism institute to be formed in partnership with Children's National Medical Center.
"Understanding the biology is interesting," she says, "but the knowledge is for a goal." Personally and professionally it's to give doctors something to zero-in on. Too often, she says, even the best intentions might amount to pulling a psychotropic drug "out of a hat" and moving down the line of antidepressants, antipsychotics, and antiepileptics to see what, if anything, sticks.
So far, nothing has for Matthew. Recently, after a frustrating 15 years of attempting treatments, he's off of prescription meds.
His doctor was willing to keep trying alternatives. But, Dr. Hu says, her son had been on medication so long she didn't even know what he was like without them. "Since we weren't seeing any strong positive effects, why not just strip it all and see what we've got?" she recalls thinking. Now he even seems to be doing a bit better.
In the meantime, she has been able to translate her dual roles into the community. Dr. Hu is the sole scientist on the board of the national capital area chapter of nonprofit Autism Speaks. "She keeps us honest," says Ann Gibbons, the chapter's executive director. "She keeps us on the straight-and-narrow scientifically, which is so important when you have a disease that is as poorly understood as autism."
The organization, she says, regularly calls upon Dr. Hu to update groups on research developments. "Our families really trust her."
And Dr. Hu's progress in the lab has buoyed the spirits of her family. "It means a lot, and it means a lot to my son," she says. "He's always said, 'Mom I think there's some good that comes out of my having Asperger syndrome, because it got you to go into autism.'"
It seems a not-uncommon thread that ties autism-related professionals to their careers. The personal connections show that "research is not being done in a vacuum," says Dr. Crawley, of the NIMH. "It's being done for a purpose, and it's being driven by real-life stories. And Valerie's is one of the best examples."
Despite any gains, Matthew still has difficulty reading social cues and interacting. He "wishes that he could take something that would help," his mother says. "So I'm constantly reading," skimming the literature for medications and treatments that seem promising.
More than anything, though, Dr. Hu's desire is simply to be able to do for him, and ultimately others, what she's been able to do over and over for anonymous Petri dishes: peek inside his cells and get a look at his genes.
"I would like to test him and see what's wrong, what pathways are faulty—then maybe there could be something pretty simple." But it's just not that easy; even a mom/scientist's hands are tied, for now, without funding or approval for a human study.
She is hopeful, though, that some day her ever-ready grant proposal to map these troubled gene pathways in human subjects will go through … and might just involve studying a population that overlaps with Matthew's age group. "As he gets older," she says with a laugh, "I have to move it up."
Until then, she says, the best treatment remains just a guess.